The Role of Genetics vs. Environment in Addiction Development
Addiction is a complex condition that affects millions of people worldwide, including individuals in Nagpur and across India. Understanding why some people become addicted while others don’t is a question that has puzzled scientists, families, and medical professionals for decades. Research increasingly shows that addiction is not simply a matter of choice or willpower. Rather, it is the result of a dynamic interaction between genetic predispositions and environmental influences.
This blog explores the roles of genetics and environment in addiction development, how they interact, and what it means for prevention, early intervention, and recovery.
Understanding Addiction
Before diving into genetics and environment, it is essential to understand what addiction is.
Addiction, also called substance use disorder (SUD), is a chronic, relapsing disorder characterized by compulsive drug or alcohol use despite harmful consequences. Addiction affects the brain’s reward system, motivation pathways, memory, and self-control. Substances such as alcohol, nicotine, opioids, cannabis, and stimulants trigger abnormal chemical changes in the brain, creating cravings and reinforcing substance-seeking behavior.
While the biological effects of substances are significant, they do not fully explain why some individuals develop addiction while others, exposed to the same substances, do not. That’s where genetics and environment come into play.
Genetics and Addiction: Nature’s Influence
Genetics refers to the hereditary factors passed down from parents to children. Studies suggest that genetic factors contribute approximately 40–60% of a person’s vulnerability to addiction. This means some individuals are biologically predisposed to develop substance use disorders due to inherited traits.
Key Genetic Factors
Dopamine Receptor Variations
Dopamine is the “feel-good” neurotransmitter that regulates pleasure and reward.
Variations in dopamine receptor genes, such as DRD2, can make the brain more or less sensitive to reward signals from substances.
Individuals with fewer dopamine receptors may seek external stimulation, like drugs or alcohol, to achieve the same level of pleasure.
Enzyme and Metabolism Genes
Genetic differences can affect how the body metabolizes substances.
For example, variations in ALDH2 or ADH1B genes can influence alcohol metabolism, affecting tolerance, sensitivity, and risk for alcoholism.
Stress Response Genes
Genes regulating the stress hormone cortisol can influence vulnerability to addiction.
People with heightened stress sensitivity may be more likely to use substances as a coping mechanism.
Impulsivity and Personality Traits
Traits such as impulsivity, risk-taking, or sensation-seeking have genetic components.
Individuals with these traits are more likely to experiment with substances and develop addictive behaviors.
Family History and Risk
A strong indicator of genetic risk is family history. Individuals with parents or siblings who have struggled with addiction are at higher risk. This does not guarantee addiction—it simply means a higher predisposition that interacts with environmental factors.
Environment and Addiction: Nurture’s Influence
While genetics provide the underlying susceptibility, environmental factors often determine whether addiction develops. Environment includes family, social circles, cultural norms, life experiences, and socioeconomic conditions.
Key Environmental Factors
Family Dynamics
Exposure to substance use at home increases risk.
Dysfunctional family environments, lack of parental guidance, or abusive relationships can trigger substance-seeking behavior.
Peer Influence
Adolescents and young adults are particularly vulnerable to peer pressure.
Friends or colleagues who normalize substance use can trigger experimentation and continued use.
Stressful Life Events
Trauma, loss, abuse, or major life transitions can drive individuals to seek coping mechanisms through substances.
Chronic stress can alter brain chemistry, amplifying vulnerability to addiction.
Socioeconomic Factors
Poverty, unemployment, and lack of education are associated with higher risk of substance abuse.
Limited access to healthcare or recreational activities can leave individuals vulnerable to addiction.
Cultural and Societal Norms
Societies that normalize alcohol, tobacco, or drug use indirectly influence initiation and maintenance of substance use.
Media portrayal of substance use can also affect attitudes and behaviors.
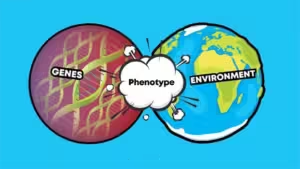
Gene-Environment Interaction
It’s important to understand that genetics and environment do not work in isolation. Rather, they interact in complex ways, determining the likelihood of addiction.
Examples of Interaction
Stress and Genetic Vulnerability
An individual with genes predisposing them to high stress sensitivity may be more likely to use substances when faced with environmental stressors.
Peer Pressure and Personality Genes
A genetically impulsive person in a high-risk social environment may experiment with drugs at an earlier age, increasing the chance of addiction.
Trauma and Neurobiological Genes
Trauma can activate genetic vulnerabilities that affect the brain’s reward and stress systems, making the individual more susceptible to substance use.
This interaction explains why some people with a strong family history of addiction never develop SUD—they may grow up in supportive, low-risk environments that counteract genetic predispositions. Conversely, individuals with minimal genetic risk may develop addiction if exposed to high-risk environments.
Epigenetics: How Environment Modifies Genes
Recent research highlights the role of epigenetics, which studies how environmental factors can change gene expression without altering the DNA sequence.
Chronic stress, trauma, or substance use can switch certain genes “on” or “off,” affecting brain chemistry and behavior.
Epigenetic changes can even be passed down to future generations, meaning environmental factors today could influence addiction vulnerability in children.
This underscores the profound interaction between nature and nurture in addiction development.
Implications for Prevention and Treatment
Understanding the interplay between genetics and environment has important implications for preventing and treating addiction.
1. Personalized Treatment Plans
Individuals with genetic predispositions may benefit from targeted therapies, such as medication-assisted treatment (MAT), alongside behavioral interventions.
2. Early Intervention Programs
Families in Nagpur can monitor at-risk individuals (e.g., those with family history) and engage in early education, counseling, and supportive interventions.
3. Environmental Modification
Reducing exposure to high-risk situations, promoting healthy social networks, and providing access to education and recreation can significantly decrease the likelihood of addiction.
4. Holistic Approaches
Combining therapy, family counseling, lifestyle interventions, and community support addresses both genetic vulnerability and environmental risk factors.
Case Study: Genetics and Environment in Action
Consider Ananya, a 22-year-old student in Nagpur. She has a family history of alcoholism, giving her a genetic predisposition. During college, she experienced stress due to academic pressure and social isolation. Her peers frequently drank at social gatherings, creating a high-risk environment.
Initially, Ananya experimented with alcohol casually, but over time, the combination of genetic susceptibility and environmental stressors led to regular use. Early recognition by her family, followed by intervention at a local Nasha Mukti Kendra, helped her understand her triggers, engage in therapy, and gradually regain control over her life.
This example illustrates how genetics set the stage, while environment determines whether addiction develops.
Conclusion
Addiction is neither solely a matter of personal choice nor purely genetic fate. It is a multifactorial condition arising from the interplay between genetic predispositions and environmental influences. Genetics provide susceptibility, while environment—family, peers, stress, culture, and trauma—shapes whether this vulnerability manifests into substance use disorder.
For families and communities in Nagpur, this knowledge is empowering:
Understanding genetic risk allows for vigilance and early intervention.
Modifying environmental factors, such as promoting supportive social networks and reducing exposure to high-risk situations, can prevent addiction.
Holistic treatment approaches addressing both genetic and environmental factors offer the best chance for sustainable recovery.
By recognizing that addiction is a complex interaction between nature and nurture, society can reduce stigma, provide better support, and help individuals lead healthier, substance-free lives.
Takeaway: Addiction is not a personal failing—it is a challenge influenced by both inherited traits and life experiences. Early awareness, supportive environments, and professional help can empower individuals to overcome substance use and reclaim their lives.




Leave A Comment